Where Does Back Pain Come From?
In 1934, William Mixter, MD and Joseph Barr, MD, established that herniation of the lumbar disc could put pressure on the nerve root or the cauda equina, resulting in sciatica. Their paper on the topic appeared in 1934 in the New England Journal of Medicine (1) and was titled:
Rupture of the Intervertebral Disc with Involvement of the Spinal Canal
Dr. Mixter was the primary author of the paper, and at the time, at age 54, he was considered to be the top surgeon in the United States. Dr. Mixter was born in 1880 and graduated from Harvard Medical School in 1906. He became a prominent surgeon at the Massachusetts General Hospital, and by 1911, along with his father, became the primary neurosurgeon at that institution. By the early 1930s, Dr. Mixter was considered to be one of the nation’s leading experts in spinal surgery, and he went on to become the first chief of the neurosurgery department at Massachusetts General Hospital.
This article by Drs. Mixter and Barr fundamentally changed the popular understanding of sciatica at that time, and for this work Dr. Mixter is generally credited by his contemporaries as being the man who best clarified the relation between the intervertebral disc and sciatica. Their landmark article helped to establish surgery’s prominent role in the management of sciatica at the time.
However, this 1934 article by Drs. Mixter and Barr did little to discuss the pathophysiology of low back pain, but rather only discussed the pathophysiology of sciatica. Drs. Mixter and Barr continued to publish studies pertaining to sciatica, and in 1941 they published in the Journal of Bone and Joint Surgery (American) (2) a paper titled:
Posterior Protrusion of the Lumbar Intervertebral Discs
In this article, Drs. Barr and Mixter continue their discussions and case series presentations of posterior lumbar spine disc protrusions and consequent sciatica. Importantly, they also offer perhaps the first explanation for reoccurring low back pain in patients who are not suffering from sciatica. They state:
“A second explanation is that a fissure occurs in the annulus fibrosus as the result of the wear and tear of ordinary use or of degenerative change, and through this fissure there is a slow, gradual extrusion of disc tissue with final resultant symptoms of sciatica when the extruded mass becomes large enough to press upon a nerve root. Clinical cases of this type may have recurring episodes of low backache over many years before the extruded mass becomes large enough to precipitate an attack of sciatica.”
In this paragraph, Drs. Barr and Mixter suggest that “recurring episodes of low backache over many years” may be the consequence of degenerative changes in the annulus fibrosus of the disc accompanied with fissures.
The modern era in the understanding of low back pain began in 1976 when internationally respected orthopedic surgeon, Dr. Alf Nachemson, published his detailed review (136 references) in the journal SPINE (3), titled:
The Lumbar Spine: An Orthopaedic Challenge
In this article, Dr. Nachemson notes that 80% of us will experience low back pain at some time in our life. He further states that:
“The intervertebral disc is most likely the cause of the pain.”
Dr. Nachemson presents 6 lines of reasoning, supported by 17 references, to support his contention that the intervertebral disc is the most likely source of back pain, including the primary research completed by Drs. MJ Smyth and V Wright in
1958 (4). Drs. Smyth and Wright published their paper in the Journal of Bone and Joint Surgery (American), titled:
Sciatica and the intervertebral disc:
An experimental study
Regarding this work by Smyth and Wright, Dr. Nachemson states:
“Investigations have been performed in which thin nylon threads were surgically fastened to various structures and around the nerve root. Three to four weeks after surgery these structures were irritated by pulling on the threads, but pain resembling that which the patient had experienced previously could only be registered only from the outer part of the annulus” of the disc.
In his 1976 review, Dr. Nachemson was noting that a non-herniated disc problem was causing back pain and that the disc itself was a probable source of back pain. Dr. Nachemson notes that the source of back pain must have a nerve supply, but at that time, good studies showing the innervation of the intervertebral disc were lacking.
Support for Dr. Nachemson’s contention of disc pain came in 1981 when Australian clinical anatomist and physician, Dr. Nikoli Bogduk, published an extensive review of the literature on the topic of disc innervation, along with his own primary research, in the prestigious Journal of Anatomy (5). Dr. Bogduk and colleagues conclude:
“The lumbar intervertebral discs are supplied by a variety of nerves.”
and
“Clinically, the concept of ‘disc pain’ is now well accepted.”
In 1983, Dr. Bogduk updates his research when he publishes an article in the journal SPINE titled (6):
The Innervation of the Lumbar Spine
In this 1983 study, Dr. Bogduk states:
“The lumbar intervertebral discs are innervated posteriorly by the sinuvertebral nerves, but laterally by branches of the ventral rami and grey rami communicantes. The posterior longitudinal ligament is innervated by the sinuvertebral nerves and the anterior longitudinal ligament by branches of the grey rami. Lateral and intermediate branches of the lumbar dorsal rami supply the iliocostalis lumborum and longissimus thoracis, respectively. Medial branches supply the multifidus, intertransversarii mediales, interspinales, interspinous ligament, and the lumbar zygapophysial joints.”
“The distribution of the intrinsic nerves of the lumbar vertebral column systematically identifies those structures that are potential sources of primary low-back pain.”
In 1986, Dr. Vert Mooney’s was the president of the International Society for the Study of the Lumbar Spine. That year, his Presidential Address was delivered at the 13th Annual Meeting of the International Society for the Study of the Lumbar Spine, May 29-June 2, 1986, Dallas, Texas. It was published in the journal SPINE in 1987, and titled (7):
Where Is the Pain Coming From?
In this article, Dr. Mooney states:
“Anatomically the motion segment of the back is made up of two synovial joints and a unique relatively avascular tissue found nowhere else in the body - the intervertebral disc. Is it possible for the disc to obey different rules of damage than the rest of the connective tissue of the musculoskeletal system?”
“Persistent pain in the back with referred pain to the leg is largely on the basis of abnormalities within the disc.”
“Mechanical events can be translated into chemical events related to pain.” An important aspect of disc nutrition and health is the mechanical aspects of the disc related to the fluid mechanics.
“Mechanical activity has a great deal to do with the exchange of water and oxygen concentration” in the disc.
The pumping action maintains the nutrition and biomechanical function of the intervertebral disc. Thus, “research substantiates the view that unchanging posture, as a result of constant pressure such as standing, sitting or lying, leads to an interruption of pressure-dependent transfer of liquid. Actually the human intervertebral disc lives because of movement.”
“In summary, what is the answer to the question of where is the pain coming from in the chronic low-back pain patient? I believe its source, ultimately, is in the disc. Basic studies and clinical experience suggest that mechanical therapy is the most rational approach to relief of this painful condition.”
“Prolonged rest and passive physical therapy modalities no longer have a place in the treatment of the chronic problem.”
The model presented by Dr. Mooney in this paper includes:
The intervertebral disc is the primary source of both back pain and referred leg pain. The disc becomes painful because of altered biochemistry, which sensitizes the pain afferents that innervate it. Disc biochemistry is altered because of mechanical problems, especially mechanical problems that reduce disc movement. Therefore, the most rational approach to the treatment of chronic low back pain is mechanical therapy that restores the motion to the joints of the spine, especially to the disc. Prolonged rest is inappropriate management.
Additional support for the disc being the primary source of back pain was presented by Dr. Stephen Kuslich and colleagues in the prestigious journal Orthopedic Clinics of North America in April 1991 (8). The title of their article is:
The Tissue Origin of Low Back Pain and Sciatica:
A Report of Pain Response to Tissue Stimulation During Operations on the Lumbar Spine Using Local Anesthesia
The authors performed 700 lumbar spine operations using only local anesthesia to determine the tissue origin of low back and leg pain, and they present the results on 193 consecutive patients studied prospectively. Several of their important findings include:
“Back pain could be produced by several lumbar tissues, but by far, the most common tissue of origin was the outer layer of the annulus fibrosis.”
The lumbar fascia could be “touched or even cut without anesthesia.”
Any pain derived from muscle pressure was “derived from local vessels and nerves, rather than the muscle bundles themselves.”
“The normal, uncompressed, or unstretched nerve root was completely insensitive to pain.”
“In spite of all that has been written about muscles, fascia, and bone as a source of pain, these tissues are really quite insensitive.”
In summary, Dr. Kuslich and colleagues found that the outer annulus is “the site” of a patient’s back pain. Irritation of a normal or inflamed nerve root never produced low back pain. Back muscles themselves are not a source of back pain; in fact, the muscles, fascia, and bone are really quite insensitive for pain. Also the inflamed, stretched, or compressed nerve root is the cause of buttock, leg pain and sciatica, but not back pain.
In 2006, physician researchers from Japan published in the journal SPINE the results of a sophisticated immunohistochemistry study of the sensory innervation of the human lumbar intervertebral disc (9). The article is titled:
The Degenerated Lumbar Intervertebral Disc is Innervated Primarily by Peptide-Containing Sensory Nerve Fibers in Humans
These authors note:
“Many investigators have reported the existence of sensory nerve fibers in the intervertebral discs of animals and humans, suggesting that the intervertebral disc can be a source of low back pain.” “Both inner and outer layers of the degenerated lumbar intervertebral disc are innervated by pain sensory nerve fibers in humans.”
Pain neuron fibers are found in all human discs that have been removed because they are the source of a patient’s chronic low back pain.
The nerve fibers in the disc, found in this study, “indicates that the disc can be a source of pain sensation.”
The perspective offered by these studies from 30 years of publications and research in the best journals is that the annulus of the intervertebral disc is primarily responsible for the majority of chronic low back pain. Acourding to Dr. Vert Mooney (7) above, the pain producing disc lesion is segmental, or pertaining to abnormal mechanical function of an intersegmental “motion segment of the back.”
Where Does Neck Pain Come From?
In 1993, Australian physician / clinical anatomist Nikioli Bogduk and American physician / radiologist Charles Aprill thoroughly evaluated the tissue sources for chronic neck pain. They published their findings in the journal Pain (10) in an article titled:
On the nature of neck pain, discography and cervical zygapophysial joint blocks
In this study, the authors evaluated the sources of chronic neck pain by using both provocation discography and cervical zygapophysial joint blocks. Their findings include:
“Both a symptomatic disc and a symptomatic zygapophysial joint were identified in the same segment in 41% of the patients.”
“Discs alone were symptomatic in only 20% of the sample.”
“Zygapophysial joints were symptomatic but discs were asymptomatic in 23%.”
“Only 17% of the patients had neither a symptomatic disc nor a symptomatic zygapophysial joint at the segments studied.”
Neck muscle injury “does not provide a satisfying model for persistent or chronic neck pain.”
A summary of the findings of Drs. Bogduk and Aprill from this 1993 study include:
The most frequent finding was “both a symptomatic disc and a symptomatic zygapophysial joint at the same segment,” seen in 41%. There is important clinical relevance to the finding that the primary source of chronic neck pain was segmental, involving both the intervertebral disc and the facet articulation.
The second most frequent finding was a symptomatic zygapophysial joint, alone, with no disc involvement, which was found in 23%.
“This indicated that 64% of the sample had a symptomatic zygapophysial joint.” [41% + 23% = 64%]
The third most frequent finding was a symptomatic disc alone, with no zygapophysial joint involvement, found at 20%.
This indicated that 61% of the sample had a symptomatic disc.
[41% + 20% = 61%]
The most important finding in this study was that the most common source for chronic neck pain was both articular (facet and disc) and segmental.
This 1993 study by Bogduk and Aprill was followed by two studies completed by the Australian research team of Leslie Barnsley, Susan Lord, Barbara Wallis, and Nikioli Bogduk. Both studies were published in the journal SPINE, in 1995 (11) and in 1996 (12). Both studies confirm the conclusions of Aprill and Bogduk from 1993: chronic neck pain is primarily segmental and articular, not muscular.
•••••
A series of experimental studies involving pigs (13, 14), cats (15) and humans (15), all published in the journal SPINE, established that sensory irritation of the nerve fibers found in the intervertebral disc and/or the facet joint capsule will initiate a reflex contraction of the segmental multifidus muscle. This has great clinical significance because the studies reviewed above document that the primary sources of chronic low back and neck pain are sensory irritations to the disc and/or facet joint capsules. Apparently the same sensory irritation causing the perception of pain also initiates a segmental contraction of the mutlifidus, locking the segmental motor unit into a fixed pattern of position and/or movement. In the chiropractic profession, this segmental locking of the motor unit is referred to as a “vertebral subluxation.”
This positive feedback loop between the disc/facet and multifidus contraction, affecting segmental motion, can explain cases of chronic spine pain. The clinical significance of this aberrant neurobiomechanics was recognized in 2006 by Dr. Manohar M. Panjabi. Dr. Panjabi, Ph.D. is from the Department of Orthopaedics and Rehabilitation, Yale University School of Medicine. A search of the National Library of Medicine database using the PubMed search engine (December 2009) showed that Dr. Panjabi is credited with an incredible 265 publications. Dr. Panjabi’s article was published in the European Spine Journal, and titled (16):
A hypothesis of chronic back pain:
Ligament subfailure injuries lead to muscle control dysfunction
In this article, Dr. Panjabi presents an explanation for chronic spinal pain as a consequence of subfailure injuries of ligaments (spinal ligaments, disc annulus and facet capsules) that cause chronic segmental muscle control dysfunction. His treatment approach is to treat the articular (disc and facet) mechanoreceptors. It appears that the positive feedback loop causing chronic segmental muscle control dysfunction can be aborted by improving segmental articular mechanical function.
How Does One Abort
the Positive Feedback Loop of Segmental Dysfunction?
Two studies show that the positive feedback loop of segmental dysfunction can be aborted by the stretching of the facet joint capsules at the level of dysfunction, resulting in the firing of facet joint mechanoreceptors. One study involved pigs, and was published in SPINE in 1997 (14). The other study involved humans, and was published in the New England Journal of Medicine in 1994 (17). In the 1997 study, stretching of the facet joint capsules and firing of the capsular mechanoreceptors aborted the contraction of the multifidus muscle. In the 1994 study, stretching of the facet joint capsules and firing of the capsular mechanoreceptors aborted the patient’s pain complaint. In both studies, the stretching of the facet joint capsules and firing of the capsular mechanoreceptors was accomplished by distending the capsule by the injection of a liquid. The exact words from the 1994 New England Journal of Medicine study were:
“… the patients who derived a benefit from either treatment may have had a condition that was improved by the stretching of the joint capsule during intraarticular injection, irrespective of what was injected.”
Can exercise initiate adequate stretch to the facet joint capsules to fire the mechanoreceptors, abort the multifitus contraction, improve segmental biomechanics and inhibit chronic pain?
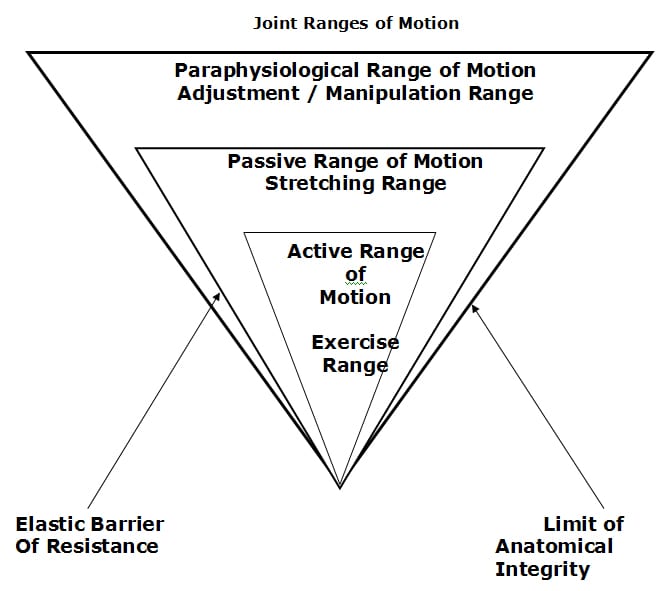
Apparently, the answer is “No,” or at least not very well. This does not imply that exercise is without value as an aspect of chronic spinal pain management. Recall from Dr. Kirkaldy-Willis that segmental motion has three ranges (18):
According to Dr. Kirkaldy-Willis, the limit of anatomical integrity is created by the capsular ligaments of the facet joints. It is the stretching of these capsular ligaments that fires the mechanoreceptors that abort the deleterious positive feedback loop discussed above. Exercise is less effective in affecting the joint capsular ligaments that other approaches.
Is there a method to stretch to the facet joint capsules to fire the mechanoreceptors, abort the multifitus contraction, improve segmental biomechanics and inhibit pain?
Apparently, the answer is “Yes.” As a representative study, in 2002, physical therapist Jan Lucas Hoving published a study in the Annals of Internal Medicine, titled (19):
Manual Therapy, Physical Therapy, or Continued Care by a General Practitioner for Patients with Neck Pain:
A Randomized, Controlled Trial
In this study, “Manual Therapy” was defined as:
“According to the International Federation of Orthopedic Manipulative Therapies, ‘Orthopedic manipulative (manual) therapy is a specialization within physical therapy and provides comprehensive conservative management for pain and other symptoms of neuro-musculo-articular dysfunction in the spine and extremities.’”
This study involved 183 patients who were followed for a 7-week period. The physical therapy used consisted primarily of active exercise, therapies exercises, postural exercises, and stretching. At 7 weeks, the success rates were 68.3% for manual therapy, 50.8% for physical therapy exercise, and 35.9% for continued physician care. The authors noted:
“The success rates for manual therapy were statistically significantly higher than those for physical therapy [exercise].”
“Manual therapy scored better than physical therapy [exercise] on all outcome measures…”
“Range of motion improved more markedly for those who received manual therapy or physical therapy [exercise] than for those who received continued care.”
“Patients receiving manual therapy had fewer absences from work than patients receiving physical therapy [exercise] or continued [physician] care.”
“Manual therapy and physical therapy [exercise] each resulted in statistically significantly less analgesic use than continued [physician] care.”
“The postulated objective of manual therapy is the restoration of normal joint motion, was achieved, as indicated by the relatively large increase in the range of motion of the cervical spine.”
“In our study, mobilization, the passive component of the manual therapy strategy, formed the main contrast with physical therapy [exercise] or continued care and was considered to be the most effective component.”
These authors concluded:
“In daily practice, manual therapy is a favorable treatment option for patients with neck pain compared with physical therapy or continued care by a general practitioner.”
“Primary care physicians should consider manual therapy when treating patients with neck pain.”
Conclusions
Chronic spine pain is often articular (disc and/or facet) and segmental. Sensory nerves in the disc and/or facet joint capsules can initiate the perception of the pain signal in the brain; and simultaneously initiate a reflex to the segmental multifidus muscle, locking the segmental motor unit into aberrant and adverse positional or movement patterns. These aberrant and adverse positional or movement patterns further stress the disc and/or facet capsule sensory nerves, creating a positive feedback loop. This adverse positive feedback loop can be aborted by the firing of facet joint capsule mechanoreceptors. The firing of the facet joint capsule mechanoreceptors can be safely accomplished with manual/manipulative therapy, improving local biomechanics, pain and disability. Such manual/manipulative therapy requires education, experience, and skill.
References
1) Mixter WJ, Barr JS. Rupture of the Intervertebral Disc with Involvement of the Spinal Canal. New England Journal of Medicine. CCXI, 210, 1934.
2) Barr JS, Mixter WJ. Posterior Protrusion of the Lumbar Intervertebral Discs. Journal of Bone and Joint Surgery (American). 1941;23:444-456.
3) Nachemson AL, The Lumbar Spine: An Orthopaedic Challenge. Spine, Volume 1, Number 1, March 1976, pp. 59-71.
4) Smyth MJ, Wright V, Sciatica and the intervertebral disc. An experimental study. Journal of Bone and Joint Surgery [American];40: 1958, pp. 1401-1408.
5) Bogduk N, Tynan W, Wilson AS. The nerve supply to the human lumbar intervertebral discs, Journal of Anatomy; 1981, 132, 1, pp. 39-56.
6) Bogduk N. The innervation of the lumbar spine. Spine. April 1983;8(3): pp. 286-93.
7) Mooney, V, Where Is the Pain Coming From? Spine, 12(8), 1987, pp. 754-759.
8) Kuslich S, Ulstrom C, Michael C; The Tissue Origin of Low Back Pain and Sciatica: A Report of Pain Response to Tissue Stimulation During Operations on the Lumbar Spine Using Local Anesthesia; Orthopedic Clinics of North America, Vol. 22, No. 2, April 1991, pp.181-7.
9) Ozawa, Tomoyuki MD; Ohtori, Seiji MD; Inoue, Gen MD; Aoki, Yasuchika MD; Moriya, Hideshige MD; Takahashi, Kazuhisa MD; The Degenerated Lumbar Intervertebral Disc is Innervated Primarily by Peptide-Containing Sensory Nerve Fibers in Humans; Spine, Volume 31(21), October 1, 2006, pp. 2418-2422.
10) Bogduk N, Aprill C. On the nature of neck pain, discography and cervical zygapophysial joint blocks; Pain; August 1993;54(2):213-7.
11) Barnsley L, Lord SM, Wallis BJ, Bogduk N. The prevalence of chronic cervical zygapophysial joint pain after whiplash. Spine. 1995 Jan 1;20(1):20-5.
12) Lord SM, Barnsley L, Wallis BJ, Bogduk N. Chronic cervical zygapophysial joint pain after whiplash. A placebo-controlled prevalence study. Spine. 1996 Aug 1;21(15):1737-44.
13) Indahl A, Kaigle A, Reikerås O, Holm S. Electromyographic response of the porcine multifidus musculature after nerve stimulation.Spine. 1995 Dec 15;20(24):2652-8.
14) Indahl A, Kaigle AM, Reikeras O et al (1997) Interaction between the porcine lumbar intervertebral disc, zygapophysial joints, and paraspinal muscles. Spine 22:2834–2840.
15) The ligamento-muscular stabilizing system of the spine. Solomonow M, Zhou BH, Harris M, Lu Y, Baratta RV. Spine. 1998 Dec 1;23(23):2552-62.
16) Panjabi MM. A hypothesis of chronic back pain: ligament subfailure injuries lead to muscle control dysfunction. Eur Spine J. 2006 May;15(5):668-76.
17) Barnsley L, Lord SM, Wallis BJ, Bogduk N. Lack of effect of intraarticular corticosteroids for chronic pain in the cervical zygapophyseal joints. N Engl J Med. 1994 Apr 14;330(15):1047-50.
18) Kirkaldy-Willis, W.H., M.D., & Cassidy, J.D.,”Spinal Manipulation in the Treatment of Low-Back Pain,” Can Fam Physician, (1985), 31:535-40.
19) Hoving JL, Koes BW, de Vet HCW, van der Windt AWM, Assendelft WJJ, van Mameren H, Devillé WLJM, Pool JJM, Scholten RJPM,Bouter LM. Manual Therapy, Physical Therapy, or Continued Care by a General Practitioner for Patients with Neck Pain A Randomized, Controlled Trial. Annals of Internal Medicine, Vol. 136 No. 10, Pages 713-722 May 21, 2002.